Verisma Prior Authorization
Free Your Practice from the Daily Burden
of physicians see prior authorization requirements on the rise1

Combined time from physicians and staff per provider to complete prior authorizations each week1
of physicians report that prior authorizations result in care delays1
The Prior Authorization (PA) process is riddled with administrative complexities, leading to delays in patient care, uncertainty in clinical decisions, and a heavy burden of paperwork. Even the most efficient practices find it challenging to complete a growing number of prior authorizations while delivering the quality of care patients deserve.
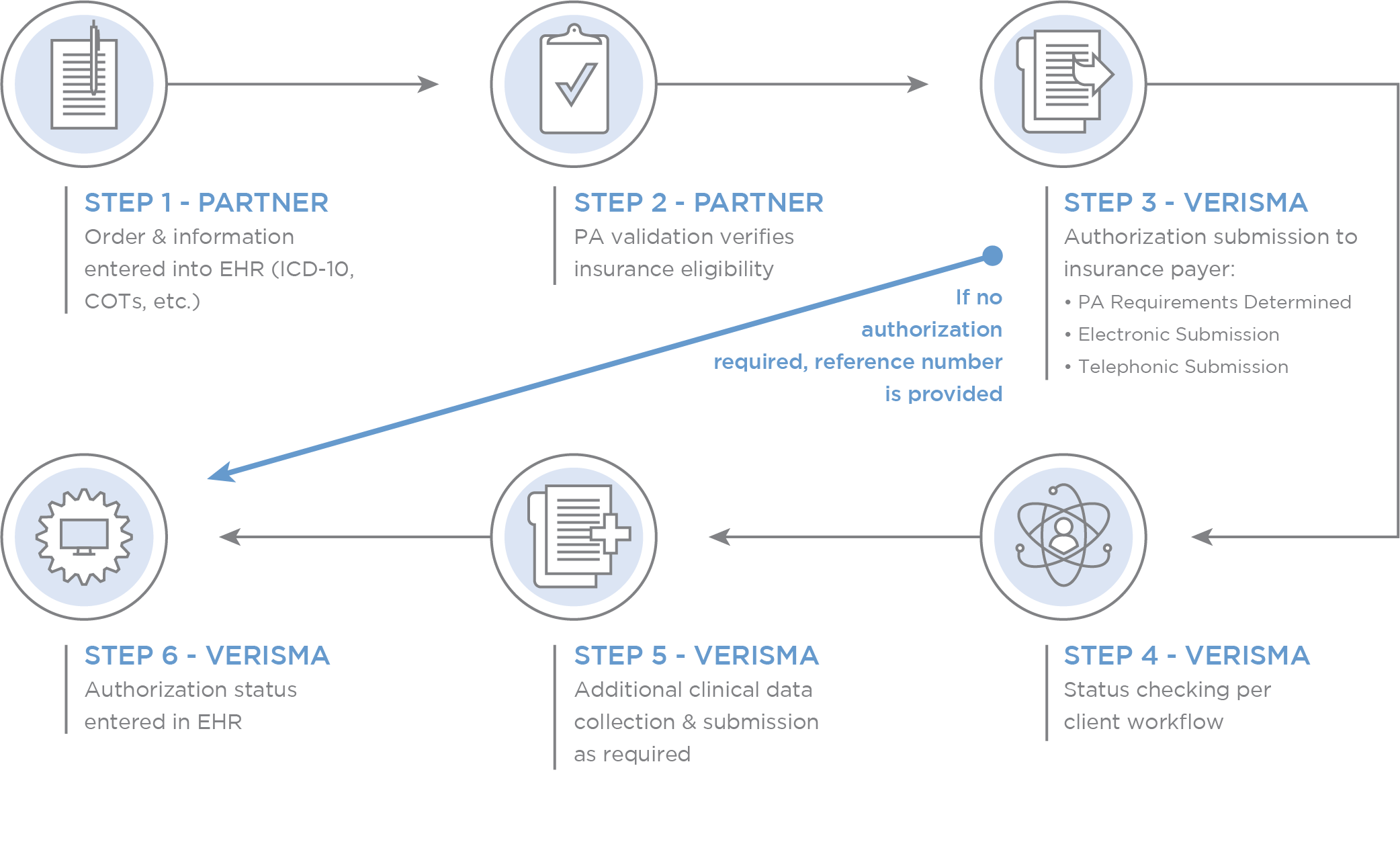
Verisma replaces a time-consuming, manual process with expertise and efficiency that simplify PAs. Our workflows are customized for each provider and executed with speed and consistency:
Benefits of Outsourcing prior authorization
- Administrative Efficiency: Reduce staff hours to complete PAs and direct clinical teams back to patient care.
- Timely Approvals: Expertise ensures that PAs are obtained as quickly as possible, minimizing treatment delays and denials.
- Standardized Criteria: Simplify the process and reduce confusion.
- Patient Trust: Preserve the patient-provider relationship with dedicated service, enuring patients feel heard and valued.
- Improved Patient Access: With less “red tape,” patients are more likely to pursue recommended treatments.
Say Goodbye to hiring, training, and managing staff
A partnership with Verisma means access to an experienced health information management team with built-in staff redundancies, internal audit layers, and compliance resources. We never call in sick, show up late, or need re-training.
With Verisma, You Can Expect:
- Tailored Solutions: Together, we’ll map, document, and optimize workflows for the unique needs of each provider.
- Transparency: We regularly report the work being done and the outcomes.
- Expertise: Verisma has a proven track record of successfully managing PAs with a high approval rate. We’re prepared to navigate shifting requirements.
- Compliance: Our staff stays updated on industry regulations to ensure PAs are fully compliant.
GET STARTED
1American Medical Association, 2018 AMA Prior Authorization Physician Survey
